Skin cancer statistics and facts in the USA
- 07 Nov, 2024

Skin cancer is the most commonly diagnosed type of cancer in the United States, with basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma being the most prevalent forms. Nonmelanoma skin cancer (NMSC), including BCC and SCC, is more common, while melanoma is a more dangerous type that can metastasize. Exposure to ultraviolet (UV) radiation, from sunlight or artificial tanning devices like tanning beds, plays a significant role in the development of skin cancer, contributing to increased melanoma and NMSC risk. It’s important to note that tanning, while darkening the skin as a protective response to UV light, does not reduce the likelihood of skin cancer development.
Other more significant risk factors are those people with a naturally pale skin color, whose skin can blister, freckle, flush or endure pain easily after sun exposure, blue or green-eyed, reddest or blond-haired, and many moles or some specific mole types. Furthermore, there are those who have been sunburnt or tanned actively, those from families with a history of skin cancer, those with a past history of skin cancer, and the old who are at risk as well.
Also geography is a contributing factor. UV light transmission is higher at greater altitudes and close to the equator because the atmosphere is thin, and the sun is at its peak in the heat. Continued exposure to X-rays and contact with arsenicals and coal increase skin cancer interface levels.
A very important preventive measure is the avoidance of certain practices, such as indoor tanning and the application of sunbathing lotions and wearing sun shields. But as surveys show, the high school students, including those surveyed through the Youth Risk Behaviour Surveillance System and the National Health Interview Survey of people over 18, exhibit different adjustments of these models depending on the age, highlighting the need for proper medication charts to monitor and address related health concerns.
Risk Factors for Skin Cancer
Several risk factors increase the likelihood of developing skin cancer, including UV exposure, genetics, and skin type. People with pale skin that burns easily, freckles, or has light-colored eyes (blue or green) are at higher risk, as well as those with red or blonde hair. Additionally, individuals with a history of frequent sunburns, tanning, or a family history of skin cancer are at increased risk. The likelihood of developing skin cancer also increases with age, as UV exposure accumulates over time. Geographical location is another factor, as regions closer to the equator or at higher altitudes tend to have stronger UV radiation due to thinner atmospheric layers. Prolonged exposure to carcinogens such as arsenicals and X-rays also heightens skin cancer risk.
Skin Cancer Prevention and Protection
One of the most effective ways to prevent skin cancer is to reduce UV exposure. Avoiding indoor tanning, wearing sun protection like SPF 15 or higher sunscreen, and protective clothing can significantly reduce the risk of skin cancer. It’s important to apply sunscreen generously and frequently, especially when outdoors for prolonged periods. Children are particularly vulnerable to sunburns and should be protected from early sun damage to reduce their lifetime risk of melanoma and other skin cancers.
Early Detection of Skin Cancer
Early detection of skin cancer can dramatically improve treatment outcomes and survival rates. Regular skin self-exams are critical for identifying changes in moles or the appearance of new skin growths, which may signal skin cancer. The "ABCDE rule" is a helpful tool for recognizing melanoma warning signs:
- Asymmetry (uneven shape)
- Border irregularities
- Color variation
- Diameter greater than 6mm
- Evolving changes, such as growth, bleeding, or itching.
Changes in moles or the emergence of new skin lesions should prompt a visit to a board-certified dermatologist for evaluation. Early-stage melanoma, when caught before it spreads, has a high five-year survival rate of 94%. However, advanced melanoma, particularly when it metastasizes to lymph nodes or other organs, has a much lower survival rate, underscoring the importance of timely detection.
Skin Cancer Treatment and Costs
Skin cancer treatment depends on the type and stage of cancer. Nonmelanoma skin cancers like BCC and SCC are highly treatable with early intervention, but melanoma requires more aggressive treatment, especially in advanced stages. Treatments include surgical excision, radiation therapy, and immunotherapies, such as immune checkpoint inhibitors and targeted therapies, which have improved survival rates. Recent advancements in melanoma treatment, particularly with the FDA approval of innovative therapies like Amtagvi (lifileucel), provide new hope for patients with metastatic melanoma who are resistant to traditional treatments. These therapies, which use the patient's immune cells to target cancer, have shown significant promise in clinical trials.
The treatment costs for skin cancer can be substantial, with the average cost for melanoma treatment estimated to be around $2,400 per patient annually. The U.S. healthcare system spends billions annually on skin cancer treatment, including a large portion of these costs attributed to NMSC and melanoma cases. In 2012-2015, over 6 million people received treatment for skin cancer, amounting to approximately $8 billion. These costs are expected to rise with increasing skin cancer cases and more advanced treatment options.
Skin Cancer Awareness and Education
Skin cancer awareness is crucial for reducing risk and improving survival rates. Awareness programs emphasize the importance of sun protection, early detection, and regular skin exams. Public health campaigns focus on preventing excessive sun exposure, using sunscreen with high SPF, and avoiding tanning beds. Education efforts also stress the risks of sunburns during childhood, as sun damage early in life significantly increases the likelihood of developing melanoma later.
Increased awareness can help people understand the risk factors, such as genetics, ethnicity, and skin type, and the importance of maintaining regular check-ups, especially for high-risk groups like individuals with a family history of skin cancer or those with many moles. Research continues to explore how lifestyle choices, UV exposure, and genetic factors influence skin cancer risk.
Skin Cancer by Age and Ethnicity
Skin cancer rates vary across different age groups and ethnicities. While skin cancer is common in older adults, melanoma in children and young adults is on the rise. Melanoma incidence rates are higher in Caucasians, especially those with fair skin, but it can also affect people with darker skin tones. Melanoma in people with darker skin is often diagnosed at later stages, making it harder to treat. Among African Americans, Hispanics, and Asians, melanoma is less common but often more aggressive when it occurs.
Skin Cancer Mortality
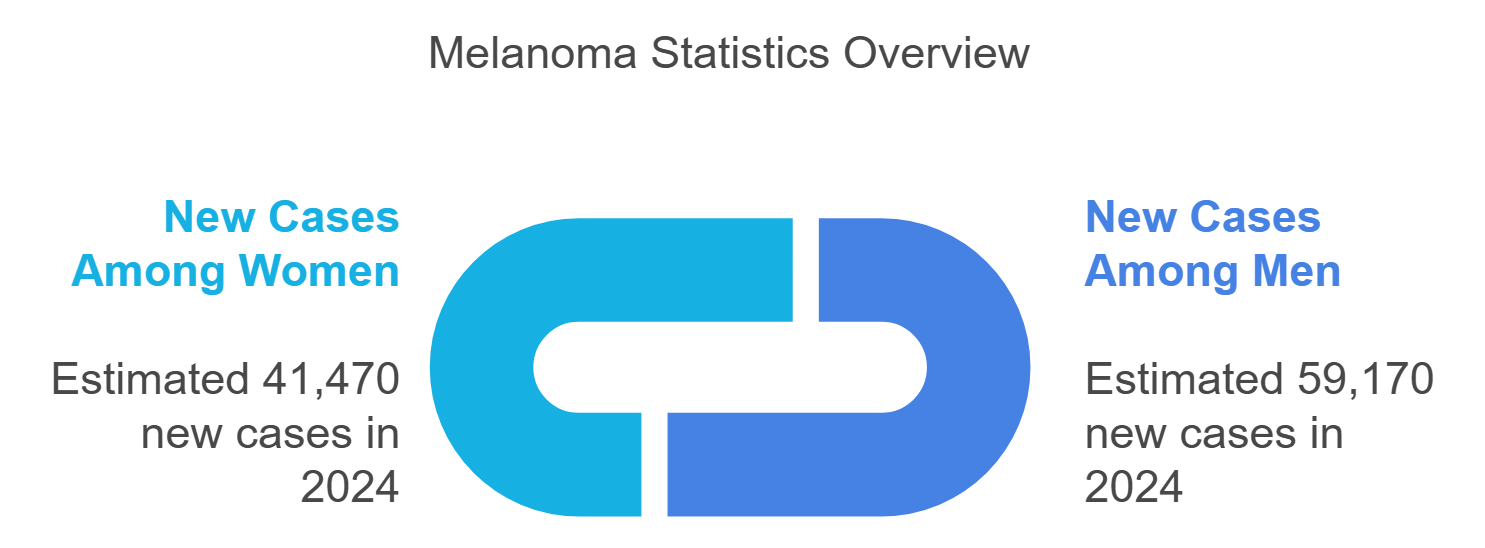
Skin cancer, particularly melanoma, is a leading cause of cancer-related death in the U.S. Nearly 20 Americans die from melanoma every day, with an estimated 8,290 deaths projected for 2024. While survival rates have improved with advances in melanoma treatment, the skin cancer mortality rate remains a serious public health concern, highlighting the need for prevention, early detection, and timely treatment.
Challenges in Management
Latest Challenges (2023)
The management of skin cancer, especially advanced melanoma, has been substantially improved with new treatment options introduced in 2023. On the sixteenth of February, Iovance Biotherapeutics’ Amtagvi (lifileucel) received approval from the Food and Drug Administration (FDA), making it a cellular therapy specifically designed for advanced skin cancers. This therapy is meant for patients suffering from metastatic melanoma and are drug resistant. These treatments employ the use of TILs or tumor-infiltrating lymphocytes whereby more immune cells are incorporated into the tumor to improve the effectiveness of treating the cancer.
What makes Amtagvi stand out from other therapies is its innovative use of the patients’ own T cells, in a fashion similar to CAR T-cell therapy. The cells are harvested, stored, and injected back into the patients to target the cancer. Following a phase 2 multi-center clinical trial, accelerated approval was granted to the therapy and its advantages are currently being confirmed in a larger phase 3 study. The therapy requires an estimated $515,000 upfront cost for each patient.
The research of Amtagvi fits well in the current trend of the treatment of melanoma headed towards the use of both immunotherapy and targeted therapy. The introduction of immune checkpoint inhibitors, drugs that lift the brakes of the immune system, greatly changed the disease prognosis, allowing even patients with advanced melanoma to experience five-year survival rates of about 50%. These treatments have changed nearly all patients who had what was previously regarded a fatal disease, into patients who can live with the disease as a chronic condition or in many cases, even get cured.
Novel Melanoma Therapies (2023)
In 2023, the most notable changes in melanoma treatment were in the adjuvant and neoadjuvant therapy management. The Food and Drug Administration approval for nivolumab (Opdivo) as an adjuvant therapy for completely resected melanoma Stage IIB/C in subjects 12 years and older is reported on October 13, 2023. The approval came after performance of the CHECKMATE-76K trial where 790 patients with Stage IIB/C melanoma were subjected to a randomized, double-blind controlled Setup. Such trial subjects were given either nivolumab at a dose of 480mg or Placebo at intravenous infusion every four weeks for either twelve months or until disease recurrence or any intolerable toxic effects was observed.
There was also a single-arm phase 2 conducted to determine the efficacy of a combination of the new drug vidutolimod and the PD-1 checkpoint inhibitor nivolumab as a therapy before surgery for patients with stage 3 cutaneous melanoma. Sponsored by the University of Pittsburgh, UPMC Hillman Cancer Center, and the National Cancer Institute (NCI), this trial documented a tumor control rate of 55 %. Published in Cancer Cell, the results endorse the further development of vidutolimod as a therapy for cutaneous melanoma but also suggests the treatment may have applicability in some other forms of cancer. It should be pointed out that this trial is the first to use this particular drug combination in the neoadjuvant setting, with effective results that are similar to approved combinations of immunotherapy.


